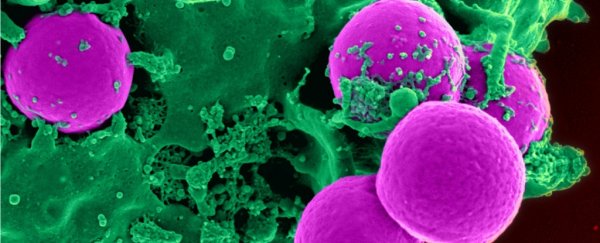
Autoimmune diseases, like type 1 diabetes and multiple sclerosis, are notoriously difficult to treat. Today, most of the therapies we've developed act indiscriminately, targeting both the healthy and unhealthy immune cells.
A new approach, tested on mice, could offer a more precise alternative that leaves patients far less vulnerable. By exclusively targeting non-functional white blood cells, the new treatment can turn off an overactive immune response - all the while leaving protective immune cells intact.
The key is a protein called programmed death 1 (PD-1), which is expressed in immune cells, like B and T lymphocytes. This protein regulates the immune system by holding back white blood cells so they can't attack the body.
While mounting evidence has shown that impaired PD-1 plays an important role in various autoimmune diseases, this is the first time it's been used as a target for therapy. And while the research is only based on mouse models so far, the authors are hopeful it will someday translate to humans.
"We are really taking treatment for autoimmune disease in a new direction," says pharmaceutical chemist Mingnan Chen from the University of Utah.
The treatment is based on a protein molecule, engineered in the lab, that targets only those immune cells with malfunctioning PD-1. This engineered molecule comes in three parts - an antibody fragment, a toxin, and a binder - and each plays a different yet equally important role.
First, the antibody fragment unlocks the impaired immune cells. Then, the toxin is released, destroying the cell from the inside out. Not to be forgotten, the binder is what keeps this molecule circulating for as long as possible.
To test this new approach, the researchers used mouse models that mimic either type 1 diabetes or multiple sclerosis (MS). In both cases, the results were extremely promising.
Not only was the treatment able to delay the onset of diabetes in mice by 10 weeks, it also halted the progression of MS-induced paralysis.
In fact, after just one dose of treatment, all six mice in the MS model regained their ability to walk, and after 25 days, the paralysis did not return.
Current therapies for MS can only delay progression, they can't reverse or cure the disease, so if paralysis can be reversed in humans using this kind of treatment, the authors say it could fill an important clinical gap.
And that goes for type 1 diabetes, too. While this new approach may only delay the onset of diabetes (and so far only in mice), the authors say if it is boosted by other treatments, the combination could hypothetically be enough to completely prevent type 1 diabetes.
Obviously, we can't get too excited just yet. This is the first time such a treatment has ever been explored, and the results are only based on mice – with no guarantees we'd see the same effect in people.
That said, the findings give us a new target to pursue.
"To make similar therapeutics for people, we would need to find the anti-human PD-1 antibody, like the anti-mouse PD-1 antibody," explains Chen.
"If we can generate the human version of therapeutics, I think we could make a huge impact in treating autoimmune disease."
This isn't some pie-in-the-sky dream, either. There are several reasons to be hopeful about the new approach.
Only a single dosage was needed to suppress autoimmunity completely, and this dosage was able to target both T cells and B cells – two common factors in autoimmune diseases. What's more, there was no long-term impact on healthy immunity in the mice studied.
As such, the authors think they have found "an effective and broadly applicable approach to treating autoimmune diseases without jeopardising healthy immunity."
The findings are reported in Nature Biomedical Engineering.