Andy Tay
Los Angeles, California, United States
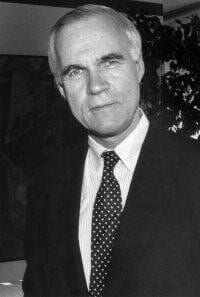 |
| Image of Lloyd Old, who is regarded as ‘The Father of Modern Tumor Immunology’, taken in 1995. He passed away on November 28, 2011 after a long battle with prostate cancer at the age of 78 years-old. Cancer Research Institute |
Cancer is a complex disease whose various causes include bacterial infections such as Helicobacter pylori leading to gastric cancer.1 Bacteria, however, can also be used to treat cancer, a treatment so effective against high grade non-invasive bladder cancer that since 1990, it has remained the preferred therapy.2
The history of using bacteria for cancer treatment can be traced to the ‘St. Peregrine tumor’. This describes spontaneous cancer regression and is named after the priest Peregrine Laziozi (1265–1345) who recovered from cancer after suffering wound infections.3 Since then, there had been several observations of cancer remission in patients infected with tuberculosis, but because these were often isolated cases, the medical community was not convinced of any correlation.4 In 1868 the German physician W. Busch noticed cancer remission in patients accidentally infected with erysipelas (skin infection) and performed a controversial experiment by moving a female cancer patient into a bed contaminated with Streptococcus pyogenes.5 His intuition was right! The cancer disappeared but the death of the woman from severe infection diminished existing interest in further the development of bacteria as anti-cancer agents.5
In 1891, the American surgeon W.B. Coley at New York Memorial Hospital learned about a patient who had a complete cancer remission after suffering from erysipelas. He hypothesized that bacterial infections could cure cancer and tested his hypothesis by infecting his patients with what is now known as Coley’s toxins—which contained Gram-positive Streptococcus pyogenes and Gram-negative Serratia marcescens.6 He achieved mixed results; some patients recovered but some patients also died from fatal infections. Subsequent clinical trials too found limited utility of Coley’s toxins.5
Between 1905 and 1918, the French tuberculosis scientists Calmette and Guérin noted that weakened tuberculosis-causing bacteria, Mycobacterium bovis, could be used as protective vaccines in cattle and monkeys. With each cycle of culturing, the virulence of the bacteria decreased.7 Learning from Coley’s experience, the pair knew that to prevent fatal infections, they had to generate weakened strains of Mycobacterium bovis. They performed sub-culture over 230 times so that the final strain could activate the human immunity without inducing exaggerated immune responses. This gave birth to modern-day Bacillus Calmette-Guérin (BCG) tuberculosis vaccine.2
Although it had been repeatedly shown that tuberculosis patients experienced lower frequency of cancer and even recovered from cancer,8 it was not until the late 1950s that BCG vaccine was tested for its anti-tumor effects. Armed with improved knowledge of immunity, Lloyd Old at the Sloan-Kettering Institute in New York made a connection between bacterial infection and stimulation of immunity for cancer fighting. In several landmark studies, he demonstrated that BCG vaccines could activate the immune system to confer resistance to transplanted tumors in mice.9 His results were supported by later independent studies, which found tumor inhibition and prevention of cancer metastasis at the site of living BCG.10 These successes motivated clinical trials of BCG as cancer therapy, and in 1969 the French scientist Mathe reported encouraging results using BCG for acute lymphoblastic leukemia.2 After more than 2500 clinical cases, BCG was finally approved for use in patients with superficial bladder cancer in 1990.2
Cancer is a challenging disease that requires a multi-pronged approach for effective intervention.1 Besides using bacteria as immune stimulators, there are recent innovations utilizing engineered probiotics like non-pathogenic Escherichia coli strain11 that seeks out hypoxic tumor environment to deliver anti-cancer drugs.12 Our fight against cancer is not expected to cease any time soon, and so our creativity and history in harnessing the power of bacteria in cancer treatments will continue on as well.
References
- Parsonnet, J. 1995. “Bacterial Infection as a Cause of Cancer.” In Environmental Health Perspectives, 103:263–68. doi:10.1289/ehp.95103s8263.
- Herr, Harry W, and Alvaro Morales. 2008. “History of Bacillus Calmette-Guerin and Bladder Cancer: An Immunotherapy Success Story.” The Journal of Urology 179 (1): 53–56. doi:10.1016/j.juro.2007.08.122.
- Hoption Cann, S A, J P van Netten, and C van Netten. 2003. “Dr William Coley and Tumour Regression: A Place in History or in the Future.” Postgraduate Medical Journal 79 (938): 672–80. URL: https://ncbi.nlm.nih.gov/pmc/articles/PMC1742910/
- Rohdenburg, G. L. 1918. “Fluctuations in the Growth Energy of Malignant Tumors in Man, with Especial Reference to Spontaneous Recession.” The Journal of Cancer Research 3 (2).
- Oelschlaeger, Tobias A. 2010. “Bacteria as Tumor Therapeutics?” Bioengineered Bugs 1 (2). Taylor & Francis: 146–47. doi:10.4161/bbug.1.2.11248.
- Jessy, Thomas. 2011. “Immunity over Inability: The Spontaneous Regression of Cancer.” Journal of Natural Science, Biology, and Medicine 2 (1): 43–49. doi:10.4103/0976-9668.82318.
- Brandau, Sven, and Henrik Suttmann. 2007. “Thirty Years of BCG Immunotherapy for Non-Muscle Invasive Bladder Cancer: A Success Story with Room for Improvement.” Biomedicine & Pharmacotherapy = Biomédecine & Pharmacothérapie 61 (6): 299–305. doi:10.1016/j.biopha.2007.05.004.
- Pearl, Raymond. Oxford Journal, 1929. “Cancer and Tuverculosis.” URL: http://aje.oxfordjournals.org/content/9/1/97.full.pdf
- Old, L J, D A Clarke, and B Benacerraf. 1959. “Effect of Bacillus Calmette-Guerin Infection on Transplanted Tumours in the Mouse.” Nature 184: 291–92. doi:10.1038/184291a0.
- Zbar, Berton, Irwin D. B., and Herbert J. R.. 1971 “Suppression of Tumor Growth at the Site of Infection With Living Bacillus Calmette Guérin.”Journal of National Cancer Institute 46 (4): 831- 839. URL: http://jnci.oxfordjournals.org/content/46/4/831.full.pdf
- Din, M Omar, Tal Danino, Arthur Prindle, Matt Skalak, Jangir Selimkhanov, Kaitlin Allen, Ellixis Julio, et al. 2016. “Synchronized Cycles of Bacterial Lysis for in Vivo Delivery.” Nature 536: 81–85. doi:10.1038/nature18930.
- Felfoul, Ouajdi, Mahmood Mohammadi, Samira Taherkhani, Dominic de Lanauze, Yong Zhong Xu, Dumitru Loghin, Sherief Essa, et al. 2016. “Magneto-Aerotactic Bacteria Deliver Drug-Containing Nanoliposomes to Tumour Hypoxic Regions.” Nature Nanotechnology 11: 941-6. doi:10.1038/nnano.2016.137.
ANDY TAY is a PhD student reading bioengineering in the University of California, Los Angeles. His research focuses on remote magnetic neural stimulation and directed evolution of magnetotactic bacteria. He has contributed multiple articles with Naturejobs Blog and Science and have also won several writing contests. He hopes to explore different ways of science communication such as through technical papers, research highlights, career blogs, science history and images.
Highlighted in Frontispiece Volume 9, Issue 4 – Fall 2017 & Volume 10, Issue 1 – Winter 2018
Spring 2017 | Sections | Science

Leave a Reply