Dealing with body aches and pains is never fun. But lower back pain may be the worst. In fact, it’s one of the most common reasons people book doctor’s appointments and call out of work, per the National Institute of Health (NIH). Luckily, there are many ways to find pain relief with the best lower back pain treatments recommended by professionals.
Treatments for lower back pain relief range from simple to complex, and the right course for you depends on how long you’ve been hurting, the severity of your pain, the location of your pain, and whether your pain is structural or muscular.
Meet the experts: Justin J. Park, M.D., a board-certified orthopedic spine surgeon with The Maryland Spine Center; Lisa DeStefano, D.O., an associate professor at Michigan State University’s College of Osteopathic Medicine; Sean Mackey, M.D., Ph.D., chief of the division of pain medicine at Stanford University; Neel Anand, M.D., professor of orthopedic surgery and director of spine trauma at Cedars-Sinai Spine Center; Rahul Shah, M.D., board-certified orthopedic spine and neck surgeon
If your back pain just started, consider slacking off, just this once. “In most cases, back pain resolves in one to two weeks,” says Justin J. Park, M.D., a board-certified orthopedic spine surgeon with The Maryland Spine Center at Mercy Medical Center in Baltimore. However, other factors, like your age and activity level, could cause back pain to last for up to six weeks, he says. People who don’t pursue extreme treatment tend to have fewer complications than those who end up rushing into invasive treatments before it’s truly necessary.
But of course, the thought of wasting over a month for your pain to subside may feel unbearable. Here, find the best lower back pain remedies to find relief fast.
At-home lower back pain treatments
1. Reach for anti-inflammatory drugs
Even as you practice patience, a non-steroidal anti-inflammatory drug (NSAID), such as ibuprofen (Motrin, Advil) or naproxen (Aleve) can help reduce back pain you’re pushing through. The research behind medicine guidelines for lower back pain finds that these may give slightly better relief than acetaminophen (Tylenol).
“Most of the time when you have back pain, it’s a muscle or ligament strain and inflammation you have is helped by an anti-inflammatory,” Dr. Park says. Over long periods, NSAIDs can cause gastrointestinal problems, so Dr. Park recommends that you don’t take them for more than 10 days without consulting your doctor.
2. Find relief through ice and heat
Break out that bag of frozen peas (or a cold pack, if you want to get fancy) for the first 48 hours after the pain sets in, and put it to use for 20 minutes a session, several sessions per day. After those two days are behind you, switch to 20-minute intervals with a heating pad.
Localized cooling shuts down capillaries and reduces blood flow to the area, which helps ease the swelling, says Lisa DeStefano, D.O., an associate professor at Michigan State University’s College of Osteopathic Medicine in East Lansing. Cold also thwarts your nerves’ ability to conduct pain signals. Heat, on the other hand, loosens tight muscles and increases circulation, bringing extra oxygen to the rescue.
3. Wear supportive shoes
Some back trouble starts from the ground up. Wearing heels can be tough on your back, and that’s especially true if you tend to wear heels for hours at a time, Dr. Park says. “It causes you to arch your back more,” he explains.
If you don’t want to give up your heels, Dr. Park recommends wearing flats or sneakers when you’re in transit and keeping your heels at work or carrying them in your bag. And, when you can, throw some flats into your regular footwear rotation instead of heels. Check out a few of our favorite podiatrist-recommended shoes below:
4. Look into getting a new mattress
How old is your bed? You may be surprised to learn that the average life span of a mattress is less than 10 years. “There’s no hard-and-fast rule,” says Sean Mackey, M.D., Ph.D., chief of the division of pain medicine at Stanford University, “but if your mattress is sagging significantly or is more than six to eight years old, I’d think about getting a new one.”
Something else to consider: A firm mattress may not do your back any favors, says Carmen R. Green, M.D., a physician at the University of Michigan Back & Pain Center. A number of studies over the years suggest that people with lower back pain who sleep on medium-firm mattresses do better than those with firm beds, she says.
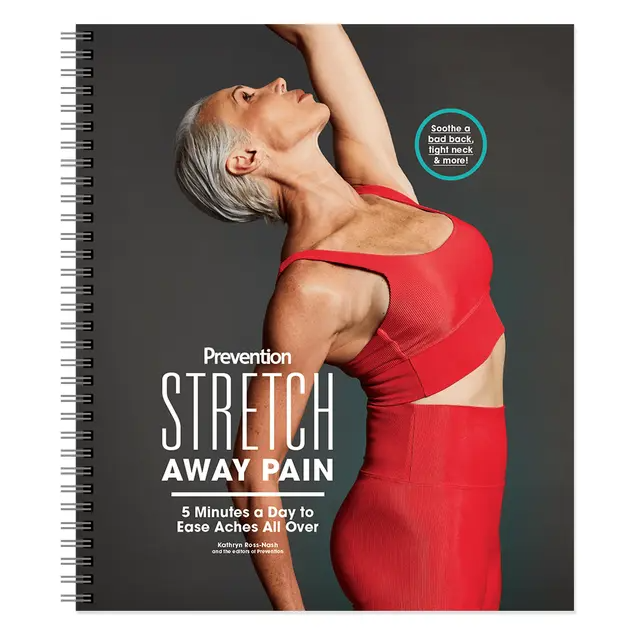
5. Do gentle stretches
Gentle stretches, walking, and periodically standing up at your desk can help stabilize your spine and prevent muscle imbalances. And despite how hard it is to imagine doing a downward-facing dog with a bad back, yoga can work in your favor, too, says Neel Anand, M.D., professor of orthopedic surgery and director of spine trauma at Cedars-Sinai Spine Center in Los Angeles.
“Not only is it almost zero impact, but the poses and stretches performed in yoga can be very therapeutic,” he says. Dr. Anand recommends stretches like cat-cow, and child’s pose to upward-facing dog to downward-facing dog. Repeat these five or more times a day, and “you just might notice some positive changes in your spine, your posture, and your overall well-being,” Dr. Anand says.
6. Focus on posture
While issues in the lower back can certainly cause poor posture, having poor posture can also cause pain. “Working on your core muscles and working on making sure that your posture is good will help you optimally load your spine and help protect your back,” explains Rahul Shah, M.D., board-certified orthopedic spine and neck surgeon.
7. Follow an anti-inflammatory diet
Following an anti-inflammatory diet has a number of potential health benefits, and while “everybody is different, in theory, it makes a lot of sense” for managing back pain, Dr. Shah explains. In fact, a 2023 study found a correlation between an anti-inflammatory diet and decreased chronic pain. There are many foods for inflammation to choose from, and Dr. Shah specifically notes that many of his patients have found success in adding turmeric to their diets.
In-office lower back pain treatments
8. Ask about prescription medications
If your back pain hasn’t resolved itself within four to six weeks, make an appointment with your doctor, who will examine your back and ask you to sit, stand, bend, walk, and lift your legs to see how your pain is affecting your mobility. You’ll likely be asked to rate your pain on a scale of one to 10, and they may do imaging tests, like an X-ray or MRI. Then, they may recommend one of the following prescribed therapies:
- Muscle relaxants: Medications like cyclobenzaprine or baclofen can help relieve painful back spasms. If you go this route, just know that side effects can include fatigue and dizziness.
- Topical pain medications: These creams and ointments, like Voltaren gel, are meant to be rubbed directly onto the area that’s hurting you.
9. Consider physical therapy
A physical therapist will teach you stretches to manage your back pain, as well as exercises to correct any imbalances that might have brought on pain in the first place. Depending on the causes and severity of your back pain, your PT may also employ other treatment techniques, such as ultrasound, electrical stimulation, and active release therapy. “Physical therapy is best for back pain when people have an episode once or twice a year,” Dr. Park says. “It helps to strengthen core muscles and back extensor muscles.”
10. Find out if injection-based treatments are right for you
If physical therapy and prescription medications aren’t working for you, steroid injections may be another option. “There are different types of shots, but what they do is coat the area [of the spine] where the nerves are. It doesn’t fix the root of the problem but it gives you some relief,” explains Dr. Shah. “Sometimes results last for a few weeks, sometimes for a few months.”
11. Experiment with acupuncture
Acupuncture may provide even more relief than painkillers, according to one 2013 review of research. In 11 studies of more than 1,100 people, this Chinese medicine staple improved symptoms of lower back pain better than simulated treatments and, in some cases, NSAIDs. The needles appear to change the way your nerves react and may reduce inflammation around joints, says Dr. DeStefano.
12. Book a massage
There’s an upside to your discomfort: It’s a legit excuse to get a weekly massage. One study found that people who did had less lower back pain and disability after 10 weeks compared with people receiving standard medical care—and general relaxation rubdowns worked just as well as structural massage targeted at specific parts of the body. Still, after a year, all the participants saw similar improvements. “My advice to patients is that if you get a massage and it helps, that’s great,” Dr. Park says. “So much of back pain is due to a muscle strain.”
13. Figure out the pain’s origin
No, the lower back pain isn’t in your head, but obsessing over it could be making it worse. “Fear, anxiety, and catastrophizing can amplify pain,” says Dr. Mackey. Because brain circuits that process pain overlap dramatically with circuits involved with emotions, panic can translate into actual pain. “Start by accepting that you have pain,” Dr. Mackey says. “Then say to yourself, it will get better.” If you struggle with overall mental wellbeing—say, you have anxiety or depression—in addition to your physical aches, it could be worth seeing a therapist to manage negative thought processes while exploring other lower back pain treatments.
14. Talk to your doctor about surgery
Back pain can be incredibly frustrating, and going under the knife may seem like the quickest, easiest fix to bring relief. But the truth is, many people don’t need surgery for lower back pain management, Dr. Park says.
“If your back pain is musculoskeletal, you will not require surgery, but if it’s a pinched nerve that’s due to a disc herniation or something else, you may need to have surgery,” he says. “But even in those people, when you go through a six-to-eight-week course of treatment that includes physical therapy and activity modification, 85 to 90% of the time, they won’t need surgery.”
However, if you try the treatments above and don’t see any improvement or still feel pain, talk to your doctor about a referral to a pain management specialist, as more specific tests or treatments may be required to get to the bottom of what’s going on.

Richard Laliberte is an award-winning veteran health journalist and former senior writer at Men's Health who writes for some of the nation's best-known magazines, blogs for WeightWatchers.com, and has authored several books.