Depression
A Hidden Cause of Resistant Depression
A third of the patients in this study shared a single vitamin deficiency.
Posted November 12, 2017
Clinical depression is distressingly common, with about 6 percent of the world population experiencing an episode at any given time, and up to 30 percent of us vulnerable to experiencing it in our lifetimes. Clinical depression is more than sadness: it's a combination of low or apathetic mood along with other physical, cognitive, and emotional symptoms that last for at least two weeks, and is on its way to becoming the most disabling medical condition in the world in the 21st century. An untreated major depressive episode can last a full year on average and strikes people in the prime of their lives.
The good news is most clinical depression is treatable. Various types of psychotherapy and/or medications can help about 60 percent of patients on the first try, and many of those who fail initial treatment eventually get better too. However, a small portion, about 15 percent, have resistant depression that lingers on and seems unresponsive to all interventions. Researchers honed in on this population in a recent study in the American Journal of Psychiatry and found that a surprising number of these very resistant cases had a single, shared metabolic abnormality.
This study took 33 patients and matched controls (excluding adolescents in the matched controls, because one of the tests, a spinal tap, was deemed too risky to do on healthy adolescents for the purposes of this study), and studied a bunch of blood, spinal fluid, and even DNA tests to see if we were missing something about the biochemistry or genetics of these folks that gave them such intractable depressive episodes. The patients were quite sick, having failed at least three medications for depression (some had failed over 10 and even electroshock therapy), most with at least one suicide attempt, and all with at least four hospitalizations. All but six had a family history of depression. Most, but not all, had depression that had begun in childhood or early adolescence.
Before we get too excited about the results, we do need to note the limitations of this study. It’s small, took place at a single medical center, and was attempted because a psychiatrist had found a metabolic abnormality in one patient with severe depression that went away with vitamin treatment. The average age of the cohort was 26, rather younger than the average age of depressed individuals. The treatment arm we’re focusing on had only 12 patients, and the treatment was open label, with no placebo control. All that said, 21 of the 33 depressed patients had metabolic abnormalities compared to zero of the matched controls. A few of the metabolic abnormalities were tracked to rare chromosomal syndromes, creatine synthase deficit, or central B12 deficiency, but 12 (or 36 percent) of these depressed patients shared a common abnormality: cerebral folate deficiency.
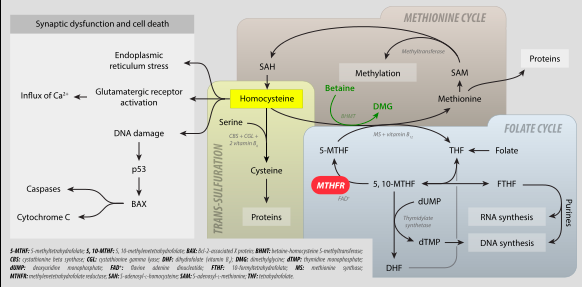
Folic acid is an essential vitamin found in food and supplements. This vitamin plays a role in all sorts of things, from making DNA to neurotransmitters. Serum folate deficiency is known to cause depression, among other problems. However, only certain forms of folic acid can get through the blood-brain barrier, so it is possible to have a completely normal folate level in the blood, but be very deficient in the central nervous system and brain. In fact, since the folic acid we get in supplements can compete at the blood-brain barrier receptor (called FR1), regular folic acid supplementation may make the problem worse. Folic acid from ordinary vitamin pills can’t get into the brain, but it can occupy the receptor, keeping the downstream folates, such as 5-MTHF, from entering the brain.
Severe cerebral folate deficiency can present in infancy as irritability, sleep disturbance, and difficulty with muscle coordination and development. Some babies even have smaller heads than usual and deafness or blindness. These children can also have autistic spectrum traits and seizures, and even schizophrenia later down the road. While some of these kids have genetic inabilities to metabolize the folate we eat into the downstream folate we use in the brain, many have antibodies to folate receptors (perhaps related to milk allergy), that keep folate from reaching the brain. Some had cerebral folate deficiency for unknown, as yet undiscovered reasons.
In the resistant depression study, of the 12 who had cerebral folate deficiency, 10 had significant improvement (including some who were cured of depression) after treatment with folinic acid, one was lost to follow up, and one didn’t take the folinic acid prescribed. All of these patients had normal folic acid and folate metabolite levels in the serum, so without the spinal tap, we wouldn’t know they had a folate problem at all. These patients also didn’t have problems with their MTHFR genes, which are now much more commonly diagnosed genetically and treated with methylfolate.
Folinic acid is an advanced folate in the folate metabolism cycle and is used in mitochondrial respiration, making DNA, and making methylfolate, which is in turn used to make neurotransmitters and to help recycle folate and methyl groups. Folinic acid rather than methylfolate is preferred in these patients because it covers problems above and beyond those with just methylfolate deficiency and can also bypass the problem of antibodies to the FR1 receptor that could underlie the deficiency in the first place.
Why do these older adolescent and young adult patients have severe depression and none of the other more overt signs of the infantile cerebral folate deficiency? Did some develop autoantibodies later or have other reasons for an acquired cerebral folate deficiency? The authors of the paper in AJP speculate that longstanding depression might even create a cerebral folate deficiency, with ongoing inflammation and excitotoxicity, with mitochondrial damage possibly using up all the cerebral folate faster than it can be replaced. All this is theoretical at the moment. The authors suggest getting a spinal tap and an accurate diagnosis before using folinic acid, as treatment will interfere with a diagnostic test, and one wouldn’t want to miss other rare inborn errors of metabolism or autoimmune diseases that might be causing the depression. In infantile cases, improvement can take as long as one to three years.
On the other hand, these preliminary studies give psychiatrists a tantalizing and impossible glimpse into practical treatments for long-suffering patients. It’s unlikely an insurance company would be willing to do expensive spinal fluid testing and metabolic work-ups for depression based on a single paper with a tiny, open label treatment arm. It would be even harder to find friendly neurologists willing to do a spinal tap, as most psychiatric offices have no tables, equipment, or expertise for that procedure. Most psychiatrists are used to thinking of resistant depression in terms of ongoing, intractable social stressors or poor coping skills or over-layered, difficult personality disorders, not biology. But we may well find that biology is the key underlying those intractable personality disorders as well, Maybe it makes sense not to have good coping skills if no coping skills have helped you, because you can't replace essential vitamins missing from the brain.
As for empirical use of folinic acid, we use methylfolate that way already. Would folinic acid be so terribly risky? Nutraceutical experts such as Jerome Sarris study folinic acid in multivitamin and mineral supplements for depression, but not near the super high doses used in cerebral folate deficiency. Those doses, however, were developed for child cases with severe neurological deficits. To get a better idea of the dosing, it would be nice to have much larger studies with a wide age range of people.
Some food for thought.
PS: I had some questions on twitter about whether we should we be supplementing grains, etc., with folic acid if it might possibly interfere with the FR1 receptors and worsen cerebral folate deficiency. Widespread folic acid supplementation has definitely decreased the incidence of neural tube defects and other sequelae of peripheral folate deficiencies. Neural tube defects were some of the most common birth defects, and they can be devastating, even fatal, so it is worthwhile trying to prevent them. However, I bet no one would have suspected cerebral folate deficiency in 1/3 of the young sample of depressed individuals above, so perhaps the frequency is more common than we thought, or perhaps the researchers just had an unusual statistical anomaly of a lot of patients in their sample. My suspicion is that for the vast majority of people, folic acid works just fine.
copyright Emily Deans MD
images from Wikimedia Commons




