We humans are very hospitable hosts: Our bodies consist of about 10 trillion cells—and each of us harbors around 100 trillion bacteria. And now, with $80, a cotton swab and a piece of toilet paper, you can discern the identity of these microscopic companions with scientific certainty. I did—and so did my mother—and scientists believe that if we can get thousands more to do so as well, we might have the data we need to hone our gut bacteria in a life-extending, internal machine.
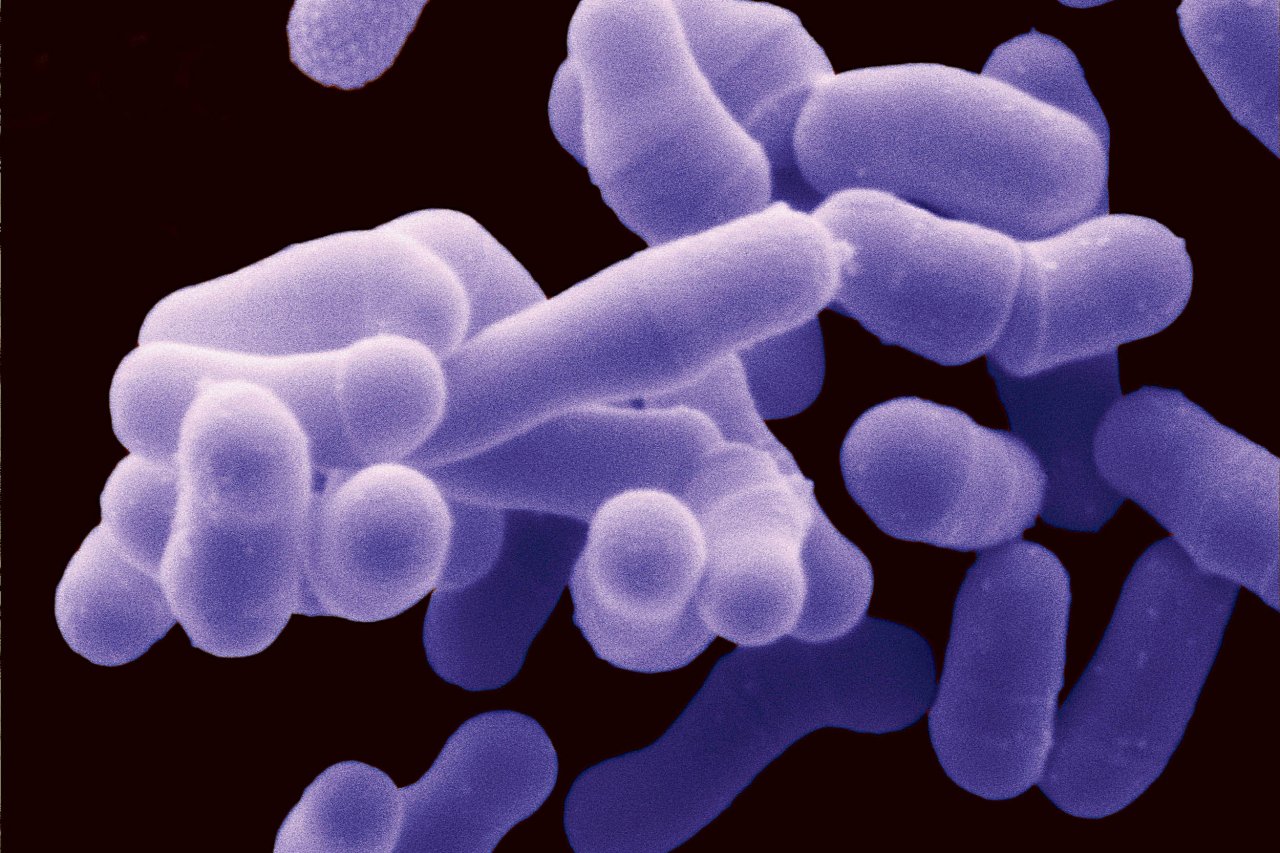
Bacteria get a bad rap. And some of them (such as Escherichia coli) can, in fact, make you ill. Yet there are also numerous bacteria that appear to promote good health, a realization that has ushered in a raft of probiotic products—from edible lubricants to chocolate to baby formula. According to one report released last year, the global probiotics market will grow from $27.9 billion in 2011 to a projected $44.9 billion in 2018.
But what does the microbiome—the vast array of microorganisms in a given environment—of a healthy gut even look like? That's the big question facing nutrition science—as well as anyone who has tried to navigate the dairy aisle and choose a probiotic yogurt in hopes of taming the ecology of his or her digestive system. To find out which microbes inhabit the intestine of a healthy individual, researchers have undertaken massive projects to sequence the DNA of the gut bacteria of various populations.
One study from 2012, for example, compared the fecal bacteria from 531 adults and children in U.S. metropolitan areas, the Amazon region of Venezuela and rural Malawi. The scientists confirmed that, among other things, babies in all three groups had gut microbiomes dominated by a group of bacteria known as Bifidobacterium. These bacteria are considered to be probiotic and are sold in the U.S. as a supplement to treat all sorts of health issues. They are also involved in the production of fermented milk products such as yogurt—a staple of Western diets—so the thinking had been that Bifidobacterium in the guts of Western babies might have come from there. This study challenged that assumption. "Finding them cross-culturally in populations where animal milk is not used suggests that they are there because of their role in digesting human milk," explains Rob Knight, one of the authors of the paper and a microbial ecologist at the BioFrontiers Institute at the University of Colorado Boulder.
Knight now wants to help you find out what organisms call your gut home. He is a senior scientist at the American Gut project, which uses direct-to-consumer marketing tactics to expand its user base, and enables regular folk to swab fecal samples (typically from the residue left on toilet paper after a wipe) and send it via snail mail for laboratory analysis. Both American Gut and a similar, competing endeavor called uBiome operate as "research projects," and for a "donation" of $99 or $89, respectively, anyone can sign up to participate. Participants sign consent forms that make the information derived from their microbiome analysis available for others to use after the data has been anonymized. The differences between the two are many and nuanced, but in essence American Gut operates as an "open-source" endeavor where data are made available for anyone to use, whereas uBiome allows access to its information to third parties only under special agreements. Both, though, have the goal of mass inclusivity.
"Right now, science is a spectator sport. I think that's limiting for humanity," says Jessica Richman, co-founder of San Francisco–based uBiome.
Richman sees a future in which companies can translate knowledge about the microbial ecology of body parts such as the gut, skin and mouth into products that promote health. "I think what is most interesting is the kinds of products that will emerge from the microbiome," she says, imagining bacteria-containing creams, for example, that people smother on their feet to prevent them from emitting offensive odors, or probiotic nasal sprays to replace antibiotics. "This could be a mainstream thing."
Intestinal Rebirth
Most people do not spend a lot of time thinking about their gut health. But that's not the case with Angela Norton, a 56-year-old teacher in Little Rock, Arkansas, who endured a life-threatening intestinal illness. In 2011 she was prescribed a course of powerful antibiotics for an abscess that had invaded her spine. The medicine treated the infection, but her gut was not the same afterward. She suffered from constant, severe diarrhea and grew so ill that she had to take disability leave from her elementary school job.
"I lost 47 pounds," Norton recalls. "I was skeletal." She sought out a gastroenterology clinic in hopes that it could diagnose what was wrong. "I was begging and pleading them to test my poop," Norton says. Finally, after a months-long odyssey, her physician ran a stool sample. It came back positive for a gut bacterium called Clostridium difficile, or C. diff.
C. diff is a nasty bacterium. It causes diarrhea so severe that, according to the Centers for Disease Control and Prevention, it is linked to 14,000 deaths in the U.S. each year. Infections with C. diff are so tough to treat that patients are increasingly turning to fecal transplants as a cure. This transplant is a somewhat crude affair in which a healthy person's stool is used to form a fecal slurry that is placed in the patient using a modified version of a colonoscopy.
Norton asked a friend from New Orleans to donate a stool sample for the procedure. Last year, the two traveled to Wisconsin to visit one of the rare clinics that offer this service. Norton was curious to find out whether the procedure would change the bacterial ecology of her gut, so she froze a sample of her stool before receiving the infusion of her friend's feces into her gut.
The fecal transplant worked. "I could tell I was better within 24 hours," says Norton.
Later, she sent a swab from the pre-transplant sample of her stool, along with one taken one month after the procedure to the American Gut project, for analysis. When the results came back, they showed that the amounts of the family Clostridiaceae—which contains some friendly strains but also includes the dangerous C. diff—had dropped from 1.6 percent in the "before" sample to undetectable levels after.
For now, it's very difficult to interpret the results of microbiome testing, which consists largely of lists of complicated scientific names of bacteria. And the researchers behind the uBiome and American Gut kits emphasize that their analyses are not meant to substitute in any way for medical diagnostics. That also means that they fall outside of the purview of the U.S. Food and Drug Administration (FDA). This is a smart maneuver because the regulatory agency has recently cracked down on companies offering direct-to-consumer genetic testing, says Nita Farahany of the Duke Institute for Genome Sciences & Policy.
In November of last year, for example, the FDA sent a warning letter to the company 23andMe telling it to "immediately discontinue marketing" of its genome sequencing products that provided information about a given individual's health risks, as this required FDA approval. Were fecal microbiome sequencing companies to start making diagnostic claims, "the FDA will care more about analytic validity," explains Farahany, and block the products until they go through the same stringent (and lengthy) approval process as medical devices.
Despite the lack of diagnostic usefulness of microbiome testing, many people such as Norton have leapt at the opportunity to sequence the bacteria living inside us. The American Gut project, which launched in late 2012, already has had 6,000 participants sign up, including the likes of author and food luminary Michael Pollan. Similarly, since the completion of a successful crowdfunding campaign concluded more than a year ago, more than 7,000 people have received uBiome kits.
Scientists such as Rob Knight believe the vast amounts of human data these projects are generating will offer clues about how gut bacteria influence our health, including our risk of allergies or autoimmune disease, and, for example, in managing our weight.
"The reason I'm convinced it's not a fad is that you can do all sorts of amazing things in mice by changing their microbiome," Knight says. For example, one study that appeared in the journal Science in September found that mice that received infusions of gut bacteria from obese humans gained about 15 percent more body fat than mice that received such bacteria from lean people.

Compare and Contrast
There is a belief in some parts of the medical community that babies delivered through vaginal birth rather than via cesarean section receive a dose of helpful bacteria from their mothers as they exit the birth canal. These babies appear to have a lower risk of developing certain ailments, including asthma and celiac disease.
I wondered how much of my gut microbiome is a manifestation of my mother's intestinal legacy, so when I logged on to the Internet and ordered a gut microbiome test on a winter day earlier this year, I enlisted my mother to do the same.
Within a week, we had received our sampling kits from American Gut (I also ordered a kit from uBiome for comparison). Really, though, our work had just begun. Both projects require you to record your food intake, so my mother and I embarked on a weeklong effort to log every meal, snack and drink that we consumed. After the week of food journaling had concluded, we sent in our samples. And waited. And waited.
The gut DNA sequencing kits can take weeks, sometimes months, to be received and analyzed. At the American Gut lab, special robotic equipment assists with the processing of samples, but issues—related to anything from problems generating enough of the DNA from the sample for sequencing to updating the visualization software that handles the data—can slow things down. There might even be a single unusual sample that uncovers a new bug, which the scientists must then take more time to account for.
When the results are finally returned, both uBiome and American Gut allow users to compare the composition of their gut microbiome results with the average results for other participants. So when I received my results I quickly logged on to see how my gut measured up.
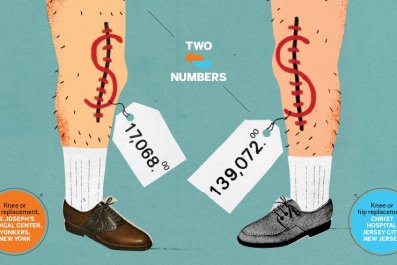
There was some bad news: uBiome told me I have about half as much Bacteroidetes bacteria in my gut as the average healthy person. Bacteroidetes bacteria "are thought to help protect against obesity because they do not digest fat well." The information could be useful, though: I started thinking I should add more red wine vinegar to my daily salad—the dressing contains polyphenols that might help tip the gut toward Bacteroidetes.
The majority of the microbes in my gut fall into a wide phylum of bacteria known as Firmicutes; these make up 74 percent of my microbiome, whereas they represent 64 percent of the microbiome of the average uBiome user. Firmicutes are a diverse bunch of bacteria thought to help with lots of things, including the digestion of fat.
My American Gut readout, however, found that Firmicutes accounted for about 65 percent of my gut bacteria (compared with around 45 percent of the average American Gut participant's readout). I'd swabbed from the same stool sample for both my American Gut and uBiome kits, so I was surprised to see my results differ. Richman, of uBiome, attributes the difference to the fact that they use different chemicals and scientific protocols for DNA extraction than the American Gut project does.
Of course the person I was most curious to compare myself against was my mother. Blame Freud, perhaps. As it turned out, my mother had a higher-than-average representation of Firmicutes in her gut as well: 60 percent. And we both registered a higher percentage than Michael Pollan, who has around 55 percent, according to information shared through the American Gut project.
More interesting, the analysis accurately indicated—based on a comparison of information in its database—that both my mother and I eat a Western diet (as opposed to that found, for example, in the Amazon or in Malawi), and predicted our ages within a decade of specificity. My mother also had about four times as much bacteria belonging to the Oxalobacter genus, which might be linked to the green, leafy vegetables that form a regular part of her meals. Best of all, Knight points out that my mother had gut microbes belonging to the Rubrivivax genus—a rare find in humans. It's previously been isolated in the fecal samples from koala bears. Beyond that, it remains a mystery as to what it really means.
"Many of the bacteria in the gut have been poorly characterized at this stage, and we are discovering more about them all the time," says Knight. "This is why projects like American Gut that look at more people are really important."
In the not-too-distant future, microbiome sequencing might become much more routine, and more detailed. Larry Smarr, an adviser to uBiome, sees endless possibilities. "I don't see why you can't have a microbiome test for your bathroom like a pregnancy test," he says—or a toilet that analyzes the bacteria from your gut after a bowel movement. The aim would be to pick up on health problems more quickly. "Monitoring the gut microbiome can detect changes which indicate beginning trends toward a disease state or indicate needed changes in the diet," Smarr explains. "You are an ecosystem, and keeping that ecosystem healthy can help keep you healthy."