Does Chronic Lyme Disease Exist?
Most patients who are diagnosed with chronic Lyme disease have prolonged somatic and/or neurocognitive symptoms, such as fatigue, arthralgias or memory impairment, but usually lack the objective findings classically associated with Lyme disease. The term 'chronic Lyme disease' implicitly suggests that these symptoms are caused by infection with B. burgdorferi, and it is often argued that infection with this organism may become persistent despite antimicrobial therapy. These assumptions, however, have not translated to any accepted clinical, pathologic or microbiologic definition of the term. One clinical practice guideline devoted to the management of chronic Lyme disease included a provisional definition so broad that Lyme disease could not be differentiated from the myriad other medical conditions (Box 2).[30] Without a definition, the term lacks meaning and it becomes fruitless to debate about whether or not 'chronic Lyme disease' exists as such.
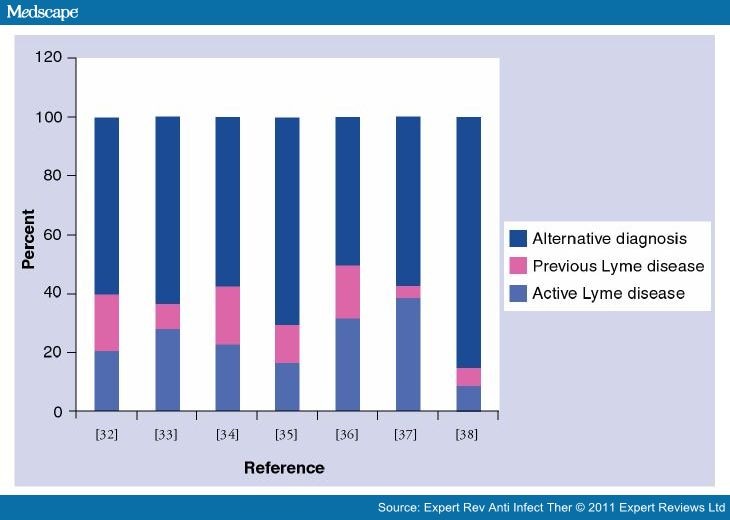
Unable to precisely say what chronic Lyme disease is, we must next examine the features of patients referred for Lyme disease to discern whether there emerges a subset who have verifiable Lyme disease, and who appear to have chronic, treatment-refractory infection. In seven studies conducted in endemic areas, comprising a total of 1902 patients referred for suspected Lyme disease, only 7–31% had active Lyme disease and 5–20% had previous Lyme disease.[31–37] Among the remainder, 50–88% had no evidence of ever having had Lyme disease (Figure 1). Most of these patients had either an alternative medical diagnosis or a functional somatic syndrome such as chronic fatigue syndrome or fibromyalgia. A substantial number were diagnosed with Lyme disease based on an inability to make an alternative diagnosis – referred to in one paper as 'diagnosis of Lyme disease by exclusion'.[36] Primary psychiatric diagnoses, psychiatric comorbidity and psychological traits such as catastrophization and negative affect are also common.[32,34] Many had symptoms of long duration and had received multiple courses of antibiotics directed at Lyme disease. Similar observations were made in Vancouver, British Columbia, where Lyme disease is very rare; of 65 patients referred for Lyme disease, 61 had either an alternative medical diagnosis or a functional somatic syndrome, and nine had a primary psychiatric diagnosis.[38]
Figure 1.
Categorization of persons referred for Lyme disease in endemic areas. Alternative diagnoses are categorized differently in the cited references, but include definite alternative medical diagnoses, chronic functional syndromes (e.g., fibromyalgia), symptomatic persons with no adequate explanation and asymptomatic persons referred because of abnormal test results.
Data taken from [31–37].
These studies underscore the degree of concern about Lyme disease in clinical practice, but even in the most highly endemic areas, less than a third of referred patients prove to have the disease in the end. The remainder appears to divide into at least three broad categories: those with alternative medical diagnoses, those with functional somatic syndromes, and a minority who have persistent symptoms that follow treatment for Lyme disease. This is true, notwithstanding the results of diagnostic testing: while a negative test may help exclude Lyme disease in patients with a low pretest probability, a positive test does not necessarily confirm the diagnosis in this scenario.[39] The positive predictive value of Lyme serodiagnostics is poor in patients with only nonspecific symptoms. Patients may coincidentally have positive Lyme serology for a variety of reasons, including asymptomatic seroconversion, generation of cross-reactive antibodies in other infectious or inflammatory diseases, or a previous treated episode of Lyme disease, and the prevalence of asymptomatic seropositivity may match or exceed the cumulative incidence of confirmed disease.[31,35,36,39–46]
Expert Rev Anti Infect Ther. 2011;9(7):787-797. © 2011 Expert Reviews Ltd.
Cite this: Chronic Lyme Disease: The Controversies and the Science - Medscape - Jul 01, 2011.











Comments